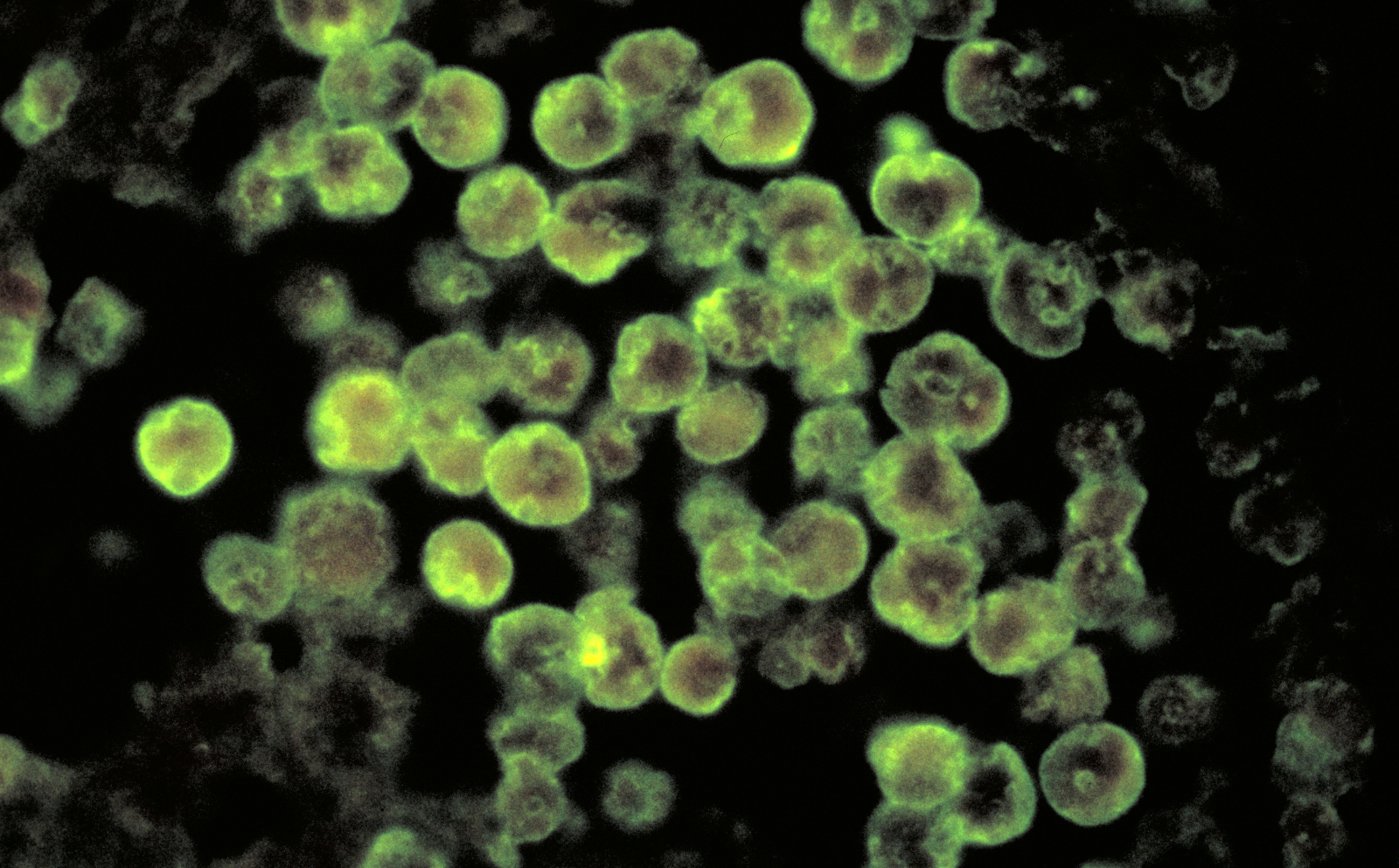
A 16-month-old boy was playing in a splash pad at a country club in Little Rock, Arkansas, this summer when water containing a very rare and deadly brain-eating amoeba went up his nose. He died a few days later in the hospital. The toddler wasn’t the first person in the United States to contract the freshwater amoeba, Naegleria fowleri, this year. In February, a man in Florida died after rinsing his sinuses with unboiled water — the first Naegleria fowleri-linked death to occur in winter in the U.S.
2023 was also an active year for Vibrio vulnificus, a type of flesh-eating bacteria. There were 11 deaths connected to the bacteria in Florida, three deaths in North Carolina, and another three deaths in New York and Connecticut. Then there was the first-ever locally transmitted case of mosquito-borne dengue fever in Southern California in October, followed by another case a couple of weeks later.
Scientists have warned that climate change would alter the prevalence and spread of disease in the U.S., particularly those caused by pathogens that are sensitive to temperature. This year’s spate of rare illnesses may have come as a surprise to the uninitiated, but researchers who have been following the way climate change influences disease say 2023 represents the continuation of a trend they expect will become more pronounced over time: The geographic distribution of pathogens and the timing of their emergence are undergoing a shift.
BSIP/Universal Images Group via Getty Images
“These are broadly the patterns that we would expect,” said Rachel Baker, assistant professor of epidemiology, environment, and society at Brown University. “Things start moving northward, expand outside the tropics.” The number of outbreaks Americans see each year, said Colin Carlson, a global change biologist studying the relationship between global climate change, biodiversity loss, and emerging infectious diseases at Georgetown University, “is going to continue to increase.”
That’s because climate change can have a profound effect on the factors that drive disease, such as temperature, extreme weather, and even human behavior. A 2021 study found water temperature was among the top environmental factors affecting the distribution and abundance of Naegleria fowleri, which thrives in water temperatures above 100 degrees Fahrenheit but can also survive frigid winters by forming cysts in lake or pond sediment. The amoeba infects people when it enters the nasal canal and, from there, the brain. “As surface water temperatures increase with climate change, it is likely that this amoeba will pose a greater threat to human health,” the study said.
Vibrio bacteria, which has been called the “microbial barometer of climate change,” is affected in a similar way. The ocean has absorbed the vast majority of human-caused warming over the past century and a half, and sea surface temperatures, especially along the nation’s coasts, are beginning to rise precipitously as a result. Studies that have mapped Vibrio vulnificus growth show the bacteria stretching northward along the eastern coastline of the U.S. in lockstep with rising temperatures. Hotter summers also lead to more people seeking bodies of water to cool off in, which may influence the number of human exposures to the bacteria, a study said. People get infected by consuming contaminated shellfish or exposing an open wound — no matter how small — to Vibrio-contaminated water.
Mosquitoes breed in warm, moist conditions and can spread diseases like dengue when they bite people. Studies show the species of mosquito that carries dengue, which is endemic in many parts of the Global South, is moving north into new territory as temperatures climb and flooding becomes more frequent and extreme. A study from 2019 warned that much of the southeastern U.S. is likely to become hospitable to dengue by 2050.

Joe Raedle/Getty Images
Other warmth-loving pathogens and carriers of pathogens are on the move, too — some of them affecting thousands of people a year. Valley fever, a fungal disease that can progress into a disfiguring and deadly illness, is spreading through a West that is drier and hotter than it used to be. The lone star tick, an aggressive hunter that often leaves the humans it bites with a life-long allergy to red meat, is expanding northward as winter temperatures grow milder and longer breeding seasons allow for a larger and more distributed tick population.
The effect that rising temperatures have on these diseases doesn’t necessarily signal that every death linked to a brain-eating amoeba or Vibrio that occurred this year wouldn’t have happened in the absence of climate change — rare pathogens were claiming lives long before anthropogenic warming began altering the planet’s dynamics. Future analyses may look at the outbreaks that took place in 2023 individually to determine whether rising temperatures or some other climate change-related factor played a role. What is clear is that climate change is creating more opportunities for rare infectious diseases to crop up. Daniel R. Brooks, a professor of evolutionary biology at the University of Toronto and author of a book on climate change and emerging diseases, calls this “pathogen pollution,” or “the accumulation of a lot of little emergences.”
State and local health departments have few tools at their disposal for predicting anomalous disease outbreaks, and doctors often aren’t familiar with diseases that aren’t endemic to their region. But health institutions can take steps to limit the spread of rare climate-driven pathogens. Medical schools could incorporate climate-sensitive diseases into their curricula so their students know how to recognize these burgeoning threats no matter where in the U.S. they eventually land. A rapid test for Naegleria fowleri in water samples already exists and could be used by health departments to test pools and other summer-time hot spots for the amoeba. States could conduct real-time monitoring of beaches for Vibrio bacteria via satellite. Cities can monitor the larvae of the mosquito species that spreads dengue and other diseases and spray pesticides to reduce the numbers of adult mosquitoes.
“If we were looking proactively for pathogens before they caused disease, we could better anticipate local outbreaks,” Brooks said. In other words, he said, we should be “finding them before they find us.”